Stress fractures are microscopic cracks in the bone. They are caused by repetitive force, often from overuse, such as jumping up and down repeatedly or running long distances. Stress fractures can also occur as a result of normal use of a bone that has been weakened by a condition like osteoporosis.
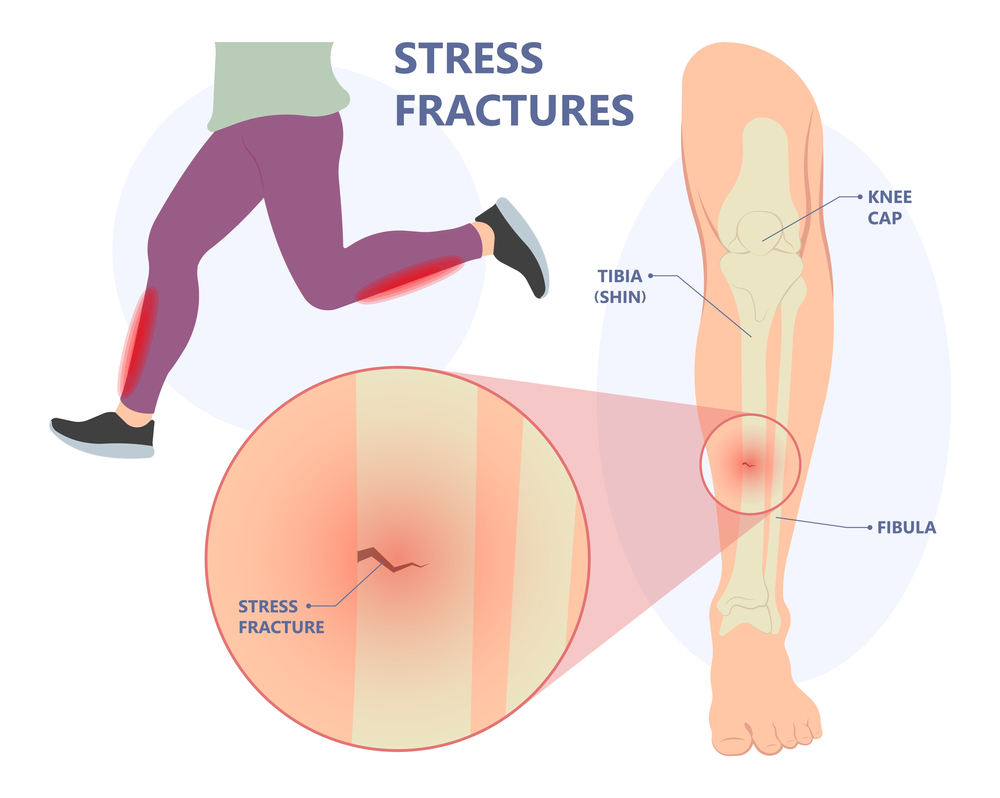
The weight-bearing bones of the lower leg and foot are the most vulnerable to stress fractures. Track and field athletes and military recruits who carry heavy packs over long distances are most at risk, but stress fractures can happen to anyone. If you begin a new exercise programme, for example, if you do too much too soon, you may develop stress fractures.
What is the difference between a stress reaction and a stress fracture?
A stress reaction is similar to a deep bone bruise that occurs as a result of trauma or overuse. Upon diagnosis, stress injuries can be classified as early (stress reaction) or late (stress fracture). A stress fracture will form if a stress reaction is not treated. A stress fracture is caused by repetitive trauma, which is usually caused by overuse. Overuse injuries account for nearly half of all sports-related injuries.
Causes of a stress fracture?
Stress fracture risk factors are classified into two types: extrinsic and intrinsic.
Extrinsic factors are those that occur outside of the body. These are also known as environmental (nature) factors. These elements may include:
- Using improper training or sport technique.
- Having a training programme or volume of activity that is too rapid, or changing your activity level without a gradual break-in period.
- Changing your exercise surface, such as going from a soft surface (such as an indoor track) to outside on gravel or concrete.
- Running on a sloped surfaced track or road.
- Using inadequate equipment or footwear (shoes that are too worn out, too flimsy or too stiff).
- Repeated activity in high-impact sports, such as long-distance running (tibia, hip).
- Having a poor diet with insufficient caloric intake for the volume of sport.
- Having a deficiency in vitamin D.
- Experiencing early sports specialization. Youth who play one sport nonstop all year are at risk of stress fractures.
Intrinsic factors are those that are specific to the athlete or patient and are not influenced by external forces. These elements may include:
Age
Older athletes may suffer from osteoporosis or other problems with their bone density. Bone that is already weakened will react to stress and/or fracture more quickly than healthy bone.
Weight
Stress injuries appear to be possible at either end of the spectrum. A person with a low BMI or who is underweight may have fragile bones, while a person with a high BMI who repeatedly loads themselves with their own weight is also at danger of suffering an injury.
Anatomy
The manner the foot lands can be affected by foot issues. These foot issues may include tendinitis, bunions, blisters, low or high arches, and bunions. Other contributing factors include muscle weakness, imbalances, and lack of flexibility.
Sex
Women who experience irregular or no menstruation may be at risk.
Medications: Osteoporosis or other illnesses that reduce bone density and strength (thickness). It’s possible that the weak or mushy bones can’t manage the variations in activity.
Symptoms of a stress fracture?
- Ache, swell, or pain at the fracture site.
- sensitivity to touch or “pinpoint pain” when the bone is touched.
- Pain that starts after beginning an activity and goes away after resting.
- persistent discomfort that lasts the entire duration of the activity and persists after it is over.
- aches and pains that come up during rest, during everyday motion, or when walking.
- Hopping on one leg makes the pain greater, as does being unable to transfer your weight or hop on the injured leg or foot.
The discomfort from a stress fracture (stress response) might get worse if it is not addressed at an early stage. Additionally, there is a chance that the fracture could shift (the fractured bone moves out of normal alignment). Hip stress fractures are examples of “high risk” stress fractures because, if not treated promptly, they may result in a bad outcome (such as requiring surgery).
Diagnosis of stress fracture
Physical examination
Your doctor will do a physical examination during your initial visit and go over your risk factors for getting a stress fracture. You will be questioned about your medical history, employment, hobbies, and any medications you may be taking while discussing risk factors.
- Magnetic resonance imaging (MRI).
- Bone Scan.
X-Rays
In order to check for a fracture, your doctor could prescribe an X-Ray. A stress fracture, however, might be challenging to detect on an X-Ray because the bone frequently looks normal and the minute breaks aren’t visible on the image. In reality, X-rays only detect roughly 2/3 of stress fractures. A stress fracture may be difficult to diagnose using X-rays unless it has already begun to heal. On X-Rays, a callus or lump that is formed when the bone begins to recover can be seen. Your doctor can suggest an imaging test that is more sensitive than an X-Ray and will detect a stress reaction even before it may develop into a stress fracture if they have a high degree of suspicion that you have a stress fracture. These examinations could consist of: Magnetic resonance imaging (MRI).
Bone scan
Stress fractures that are invisible on an X-Ray may be seen using a bone scan. A tracer, a radioactive material, is put into your bloodstream during a bone scan. In the places where the bone is being healed, the tracer settles and accumulates in the bone. On the bone scan, the stress fractured area will be visible as being darker than the uninjured area.
Magnetic resonance imaging (MRI)
An MRI may be done if your doctor wants extremely precise imaging of the damage. A huge magnet, radio waves, and a computer are used in the magnetic resonance imaging (MRI) test to provide extremely sharp images of the human body.
There is no radiation exposure, hence an MRI is frequently preferable.
- Compared to other imaging examinations, it takes less time.
- It is more effective at determining the nature of various bone and/or soft tissue issues.
Treatment for stress fractures
Non-surgical treatment
It’s crucial to visit your doctor since, if left untreated, the bone could entirely break. In the interim, adhere to the RICE recommendations:
- Rest- Do not engage in weight-bearing exercises. If necessary, put on supportive shoes with a stiff sole.
- Ice- Ice the region for 24 to 48 hours to reduce swelling. Apply an ice pack for 20 minutes at a time while wrapping it in a towel. Never apply ice to your skin directly.
- Compression- To reduce swelling, encircle the region with a gentle wrap.
- Elevation- Raise your leg or foot above your heart by using pillows.
Surgery for stress fractures
Severe stress fractures that do not heal on their own may necessitate surgery. Typically, fasteners such as pins, screws, plates, or a combination of these will be inserted by the doctor to hold the small bones of your foot and ankle together.
Conclusion
The implant used in skull fracture surgery determines the outcome of the procedure. As a result, Zealmax Ortho develops and sells the most dependable orthopedic implants, which have a high success rate and are widely used in surgery around the world. We offer a diverse range of bone implants at competitive prices without sacrificing quality.

