Shoulder pain and discomfort can significantly affect one’s quality of life, limiting daily activities and even hindering productivity. Fortunately, medical advancements have led to the development of minimally invasive procedures like shoulder arthroscopy, which offer effective solutions for various shoulder conditions. In this comprehensive guide, we will delve into the world of shoulder arthroscopy, exploring its procedure, benefits, and applications.
What is Shoulder Arthroscopy?
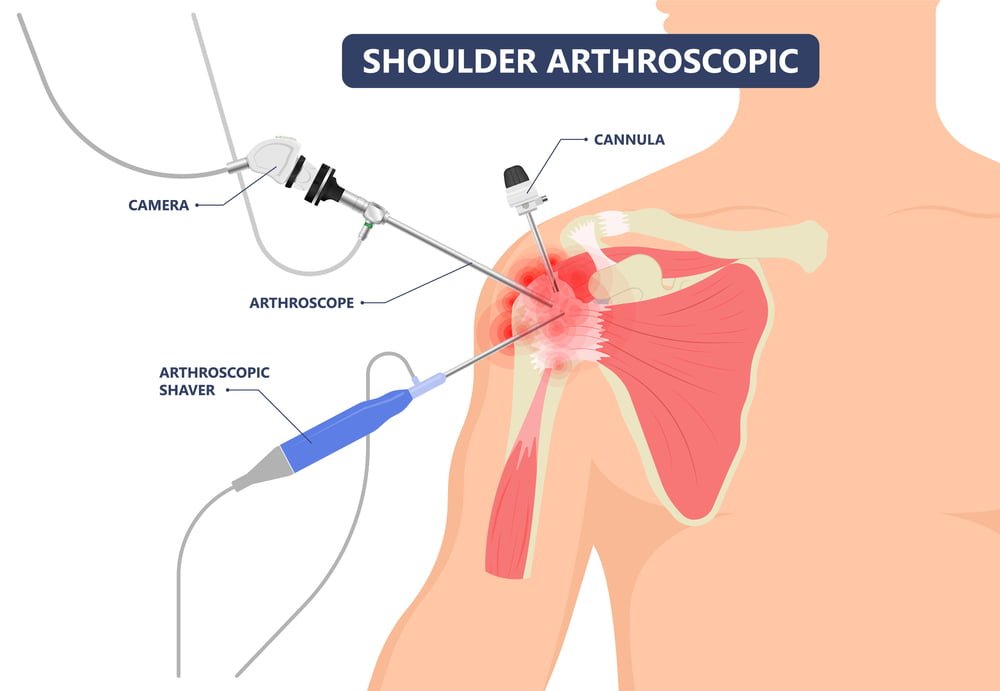
Shoulder arthroscopy is a minimally invasive surgical technique used to diagnose and treat various shoulder problems. It involves the use of a tiny camera called an arthroscope and specialized surgical instruments to access the shoulder joint through small incisions. The arthroscope transmits real-time images of the inside of the joint to a video monitor, enabling the surgeon to visualize and treat the problem.
The Procedure:
Anesthesia: Before the procedure, the patient is given either general anesthesia or regional anesthesia to numb the shoulder area.
Incisions: The surgeon makes small incisions around the shoulder joint to insert the arthroscope and other surgical instruments.
Visualization: The arthroscope is inserted, allowing the surgeon to explore the shoulder joint and identify the cause of the problem.
Treatment: Based on the findings, the surgeon can perform various procedures, such as repairing torn ligaments, removing bone spurs, or smoothing damaged cartilage.
Closure: Once the treatment is completed, the incisions are closed with sutures or adhesive strips, and a sterile dressing is applied.
Benefits of Shoulder Arthroscopy
- Minimally Invasive: Shoulder arthroscopy is considered a minimally invasive procedure compared to traditional open surgery. Instead of large incisions, only small keyhole incisions are made around the shoulder joint. This approach results in less tissue damage, reduced scarring, and minimized disruption to surrounding structures. The smaller incisions also mean that there is less bleeding during the procedure, reducing the risk of complications.
- Accurate Diagnosis: The arthroscope used in shoulder arthroscopy provides a clear and magnified view of the shoulder joint. The camera attached to the arthroscope transmits high-definition images to a video monitor, allowing the surgeon to examine the joint in detail. This visualization helps in accurate diagnosis as the surgeon can identify the exact cause of the shoulder problem, such as a torn ligament, damaged cartilage, or inflamed tissue. With a precise diagnosis, the surgeon can plan and execute appropriate treatment strategies.
- Customized Treatment: Shoulder arthroscopy allows for a wide range of procedures that can be tailored to each patient’s specific condition. The surgeon can use specialized instruments to repair torn ligaments, trim or remove bone spurs, remove damaged cartilage, and even reconstruct ligaments or tendons. The ability to customize the treatment approach ensures that patients receive individualized care, addressing their unique shoulder issues effectively.
- Faster Recovery: Due to the smaller incisions and reduced tissue trauma associated with shoulder arthroscopy, patients often experience less pain and swelling compared to traditional open surgery. The smaller incisions also mean that there is less disruption to the surrounding muscles, tendons, and ligaments, which can contribute to a shorter rehabilitation period. Additionally, the decreased postoperative pain allows for earlier initiation of physical therapy, promoting faster recovery and return to normal activities.
- Outpatient Procedure: In many cases, shoulder arthroscopy can be performed as an outpatient procedure, meaning patients can return home on the same day as the surgery. This is because the procedure is less invasive and generally associated with minimal complications. Being an outpatient procedure reduces the need for an overnight hospital stay, allowing patients to recover in the comfort of their own homes. It also eliminates the potential risks and inconveniences associated with a hospital stay.
Conditions Treated with Shoulder Arthroscopy:
Shoulder arthroscopy can effectively address a variety of shoulder conditions, including:
- Rotator Cuff Tears
- Labral Tears (SLAP Tears)
- Shoulder Impingement Syndrome
- Shoulder Instability (Dislocations)
- Frozen Shoulder (Adhesive Capsulitis)
- Biceps Tendon Disorders
- Arthritis and Joint Inflammation
Orthopedic Implants Used in Shoulder Arthroscopy
Orthopedic implants used in shoulder arthroscopy vary depending on the specific procedure and the surgeon’s preference. Here are some common types of implants used in shoulder arthroscopy:
Anchors
Anchors are small devices that are inserted into the bone to secure soft tissues like tendons or ligaments. They typically have sutures attached to them, which are used to repair and reattach damaged tissues. Anchors can be made of metal or bioabsorbable materials.
Suture materials
Various types of sutures may be used during shoulder arthroscopy, depending on the specific procedure and the surgeon’s preference. These sutures are used to repair torn or damaged tissues. Suture materials can be non-absorbable (e.g., polyester or braided polyethylene) or absorbable (e.g., polyglycolic acid or polylactic acid).
Labral repair devices
The labrum is a ring of cartilage that lines the shoulder socket. If the labrum is torn or damaged, it may need to be repaired during arthroscopy. Labral repair devices are used to reattach the torn labrum to the shoulder socket. These devices can be suture anchors or specialized implants designed for labral repair.
Glenoid resurfacing implants
In cases of severe glenoid (shoulder socket) wear or damage, glenoid resurfacing implants may be used. These implants are used to replace the damaged or worn-out glenoid surface, providing a smooth and functional joint.
Proximal humeral fracture fixation implants
Shoulder arthroscopy can also be used to treat proximal humeral fractures, which occur near the shoulder joint. In these cases, implants such as screws, plates, or intramedullary nails may be used to stabilize the fractured bone and promote proper healing.
Material Types Used In Implants
Metals:
- Stainless Steel: Strong, durable, and corrosion-resistant. Used in screws, plates, and nails.
- Titanium: Lightweight, biocompatible, and strong. Used in joint replacements, plates, and screws.
- Cobalt-Chromium Alloys: High strength and corrosion resistance. Used in joint replacements, like femoral heads.
Bioabsorbable Materials:
- Polylactic Acid (PLA) and Polyglycolic Acid (PGA): Biodegradable implants used when long-term stability isn’t required, such as in fractures or soft tissue repairs.
- Poly-L-Lactic Acid (PLLA): Provides structural support during healing and gradually degrades.
Ceramics:
- Alumina and Zirconia: Biocompatible and wear-resistant ceramics used in joint replacements, especially femoral heads.
- Calcium Phosphate Ceramics: Bioactive ceramics that promote bone growth and integration. Used in bone graft substitutes and coatings on metal implants.
Polymers:
- Polyethylene: Durable and wear-resistant polymer used in joint replacements, particularly acetabular liners.
- Polyether Ether Ketone (PEEK): High-strength polymer with excellent mechanical properties. Used in orthopedic implants like spinal fusion cages.
Conclusion
The choice of implant depends on the injury, age, activity level, and overall health of the individual. Zealmax Ortho offers orthopedic implants that are biocompatible, ensuring they are made from materials safe for the body without causing adverse reactions. These implants are designed to be durable and long-lasting, facilitating healing and restoring shoulder function following arthroscopy.

