Your jawbone supports your teeth and facilitates speaking, chewing, and swallowing. It is made up of a lower jawbone (mandible) and an upper jawbone (maxilla) (mandible). The lower jawbone is movable in all directions, but the upper jawbone is immobile. The skeletal system includes the jawbone.
Accidents and injuries frequently result in broken jaws. You may also have fractures in other parts of your face, but these fractures mostly affect your lower jaw or mandible. A temporomandibular joint pops open to reveal a displaced jaw (TMJ). Some dislocated or fractured jaws require only minimal care to heal. You might need to have your jaw wired shut for a few weeks with severe jaw injuries.
What is a mandibular fracture?
The jawbone can fracture like other bones in the body do (broken bone). The jawbone can also be dislocated. A dislocation occurs when the lower jawbone slips out of one of the two TMJs, which link the mandible to the skull.
Both disorders can be painful and make speaking and eating difficult or impossible. A fractured or dislocated jaw might also impact breathing. These medical emergencies need for immediate assessment and care.
The lower jawbone is the most commonly affected by a fracture or dislocation. Fractures can occur in the following areas:
- The part that holds your teeth in place (body).
- The angle at which your jaw curves.
- The top of the jawbone has a knob-shaped joint (condyle).
- The point at which the two sides of the lower jawbone meet (symphysis).
An upper jawbone fracture is frequently associated with facial fractures such as the cheekbone (zygomaticomaxillary or ZMC fracture) or the eye socket (orbital fracture). Broken jaws are the second most common type of facial fracture, after broken noses.
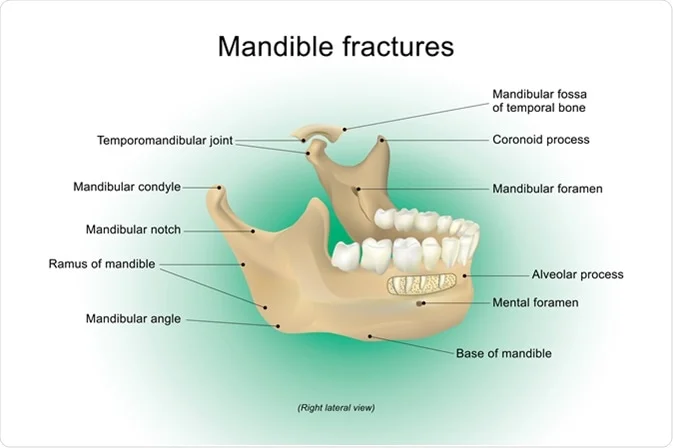
Anatomy of the Mandible
The lower jaw, or mandible, is shaped like a horseshoe, with the ends flattened and projecting upward. The mandible’s horizontal arch holds teeth and blood vessels and is thick in the front, forming the chin. The evolution of the chin is unique to humans and not found in great apes. Human ancestors, such as bonobos, have chins.
The mandible projections are attached to the temporal bone on the sides of the head. These projections are known as Rami, and they also support the chewing muscles.
Symptoms of mandibular fractures
A mandibular fracture is similar to a bone fracture in any other part of the body. The bone becomes stressed, usually as a result of excessive force, and breaks as a result of that pressure. Mandible fractures can also be caused by violence. According to a study published in the journal Seminars in Plastic Surgery, the majority of adults in the United States have experienced such trauma as a result of a violent act.
Among the symptoms of a jaw fracture are:
- In the jaw or ear area, there may be a pain, swelling, redness, and increased heat.
- Speaking, chewing, and breathing difficulties.
- Face and neck numbness or bruising.
- Loose teeth or a shift in tooth alignment.
- The mouth is bleeding.
If you suspect you have a broken mandible, see a medical or dental professional as soon as possible for a diagnosis.
What is the cause of a broken jaw?
The most common causes of broken jaws are:
- Vehicle accidents, workplace accidents, and falls are all examples of accidents.
- Assaults and injuries.
- Injuries from sports or other activities.
- What is the cause of a dislocated jaw?
- TMJ disorders and conditions that cause loose tissues and joints (such as Ehlers-Danlos syndrome) may increase the risk of jaw dislocation.
It is also possible to dislocate a jaw while doing the following:
- Having a dental procedure performed.
- Too wide of a mouth opening.
- Vomiting.
- Yawning.
What are the common causes of a broken jaw?
The following are the causes of mandibular jaw fracture:
- Fights: Because the mandibular jaw is the most common target of attack during a fight, assaults or fights are the most common cause of mandibular jaw fracture.
- Workplace accidents: Workers in industries are at a high risk of mandibular jaw fracture.
- Sports injuries: Aggressive sports such as boxing, rugby, and football increase the risk of mandibular jaw fracture.
- Accidents on the road.
Mandible fractures diagnosis
Following a physical examination of your jaw and face, you will have a radiograph taken to detect any jaw fractures caused by the injury. Maxillofacial radiologists examine dental radiographs to determine the presence and severity of cracks, splits, or complete breaks.
According to a report published in the Journal of Oral and Maxillofacial Radiology, two types of radiographs are best for identifying mandibular fractures:
CT Scan
A special type of radiograph known as cone-beam computer tomography (CBCT) allows maxillofacial radiologists to accurately assess bone conditions and fractures in three dimensions. Because you may have more than one fracture, it is critical to identify all fractures.
X-ray
A panoramic X-ray is a less expensive option that can detect 86 percent of mandibular fractures.
If you live in a community without this radiographic equipment, you may be subjected to a standard CT scan or X-ray at first. However, you will benefit from scheduling a CBCT scan before beginning treatment.
Treatment of mandible fractures
The severity of the injury determines the treatment for a broken jaw. Mild fractures may heal by themselves. While the jawbone heals, you’ll need to eat a soft or liquid diet.
More severe fractures necessitate surgery. Your doctor or nurse practitioner may:
- For several weeks, wire the upper and lower jawbones together to keep the broken bones in place.
- Apply metal plates to the fractured area to aid in bone healing and fusion.
Treatment options for a fractured mandible range from a soft diet alone to maxillomandibular fixation (wiring the jaw shut), rigid open fixation, or both. If fixation is available within a few hours of the injury, any lip or oral lacerations should be closed after the fracture has been reduced. Metal bars (arch bars) are attached to the buccal surface of the upper and lower teeth and then wired to each other after proper occlusion is established for maxillomandibular fixation. In case of vomiting, patients with maxillomandibular fixation should always carry wire cutters. Although early mobilization is usually preferred, fixation may require several weeks. Liquids, pureed foods, and supplements are the only foods allowed.
Because only a portion of the tooth surfaces can be brushed, plaque, infection, and halitosis are controlled by a 60-second rinse with 30 ML of chlorhexidine 0.12% every morning and evening. After fixation is removed, jaw-opening exercises can usually help restore function.
Condylar fractures may only require 2 to 3 weeks of maxillomandibular fixation and a soft diet. Open reduction and fixation may be required for severely displaced, bilaterally fractured condyles. Condylar fractures in children should not be immobilized rigidly because they can lead to ankylosis and abnormal facial development. 5 to 10 days of flexible (elastic) fixation is usually sufficient.
Conclusion
Zealmax Ortho is a supplier and manufacturer of orthopedic and maxillofacial implants of the highest caliber. Experts at Zealmax Ortho have been creating high-quality, reasonably priced implants to assist medical professionals in treating orthopedic disorders and injuries brought on by mandibular fracture for many years.

