The pelvis is a strong ring of bones at the base of the spine. Pelvic fractures are uncommon, accounting for only about 3% of all adult fractures. The majority of pelvic fractures are caused by a traumatic, high-energy event, such as a car accident. Because the pelvis is so close to major blood vessels and organs, pelvic fractures can result in extensive bleeding and other injuries that necessitate immediate medical attention. A lower-impact event, such as a minor fall, may be enough to cause a pelvic fracture in an older person with weaker bones.
The severity of the injury determines the treatment for a pelvic fracture. While lower-energy fractures can often be treated conservatively, surgery to reconstruct the pelvis and restore stability so that patients can resume their daily activities is usually required for high-energy pelvic fractures.
Anatomy of Pelvis
The pelvis is a ring of bones located at the trunk’s lower end, between the spine and the legs. The sacrum (the large triangular bone at the base of the spine), coccyx (tailbone), and hip bones are all part of the pelvic bones.
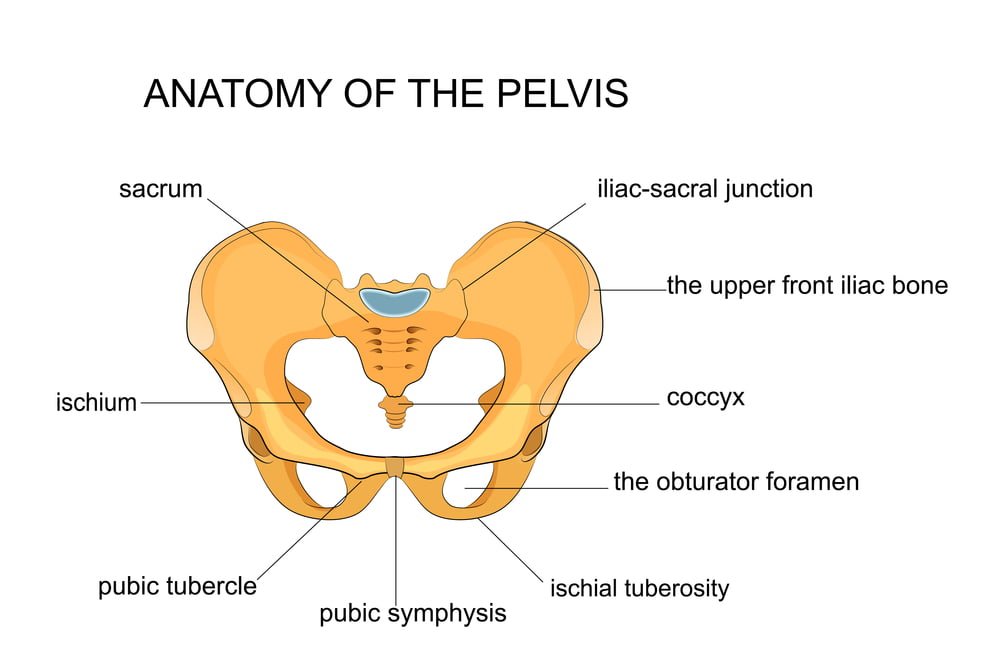
Each hip bone has three bones: the ilium, ischium, and pubis, which are separate in childhood but fuse together as we get older. The acetabulum—the hollow cup that serves as the socket for the ball-and-socket hip joint—is formed when these three bones come together.
Ligaments, which are bands of strong connective tissues, connect the pelvis to the sacrum, creating a bowl-like cavity below the rib cage.
The pelvic ring houses major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs. The pelvis protects these vital structures from harm. It also acts as an anchor for the hip, thigh, and abdomen muscles.
Types of pelvic fractures
There are many different kinds of pelvic fractures because your pelvis is made up of several bones. According to the pattern of the break, there are generally several different types of bone fractures, including:
Open or closed (compound) fractures
A closed fracture is one that doesn’t cause the skin around it to split open. A broken bone is said to have an open fracture or compound fracture if it pierces your skin.
Complete fractures
When your bone splits in half, you have a complete fracture.
Displaced fractures
A displaced fracture is when a gap develops where your bone was broken.
Partial fractures
Fractures that don’t penetrate your bone completely are referred to as partial fractures.
Stress fractures
A stress fracture occurs when a crack develops in your bone.
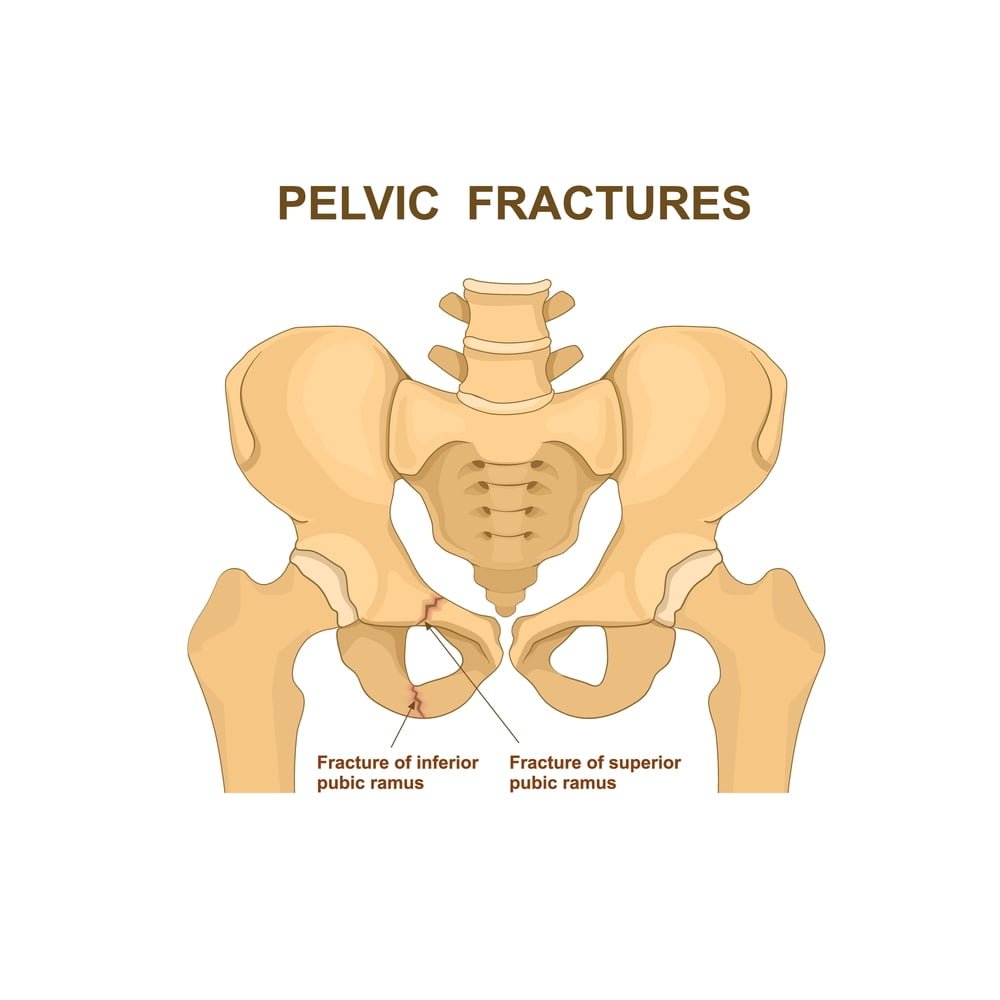
A pelvic fracture can be classified as stable or unstable in addition to the specific pattern it has:
Stable pelvic fracture
A stable pelvic fracture occurs when there is typically only one break in the pelvis and no displacement of the broken bones. Low-impact injuries to the pelvis, like a minor fall or running, typically result in stable fractures.
Unstable pelvic fracture
In an unstable pelvic fracture, the broken ends of the bones are frequently displaced and there are frequently two or more breaks. High-impact situations like a car accident are most frequently to blame for unstable pelvic fractures.
Avulsion fractures are a different kind of pelvic fracture, though they’re less frequent. A tendon or ligament that is attached to a bone tears away from the bone, taking a small piece of the bone with it. This is known as an avulsion fracture.
Occurrence of pelvic fractures and its effect
Pelvic fractures are not frequently seen. Pelvic fractures only account for 3% of adult bone fractures. The majority of pelvic fractures result from traumatic incidents like car accidents or significant falls.
A pelvic fracture can happen to anyone at any age. Older people are more likely to have mild pelvic fractures because they are more likely to have bone-weakening diseases like osteoporosis. Most severe pelvic fractures occur in patients between the ages of 15 and 28. Men are more likely than women to sustain a pelvic fracture before the age of 35, and women are more likely after the age of 35.
Signs and symptoms of a pelvic fracture
It hurts almost always when there is a stable pelvic fracture. It is common to experience hip or groin pain, which is aggravated by hip movement or walking, though it may still be possible to do so. Some patients discover that if they keep one hip or knee bent, the pain subsides.
The severity of additional symptoms varies. They may consist of:
- Groin, hip, lower back, buttock, or pelvis pain and tenderness.
- Over the pelvic bones, there is swelling and bruising.
- Upper thighs or the genital region experiencing numbness or tingling
- Pain that could also be felt when sitting and going to the bathroom.
There might also be outward indications of bleeding. There are several locations where bleeding can spread to the skin, some of which are more likely to be noticeable than others. They consist of:
- Bruising over the actual pelvic bones.
- Bruises or a sore lump on the perineum or in the groin.
- The small of the back is bruised.
- Bruising to the scrotum and vaginal bleeding in men.
- Urinary blood or blood coming from the back passage.
Possible causes of pelvic fractures
High-impact events
Since your pelvis is a very stable bone structure, high-impact incidents like a car accident or a significant fall are the main causes of pelvic fractures. Unstable pelvic fractures are typically the result of high-impact events.
Bone-weakening diseases
Pelvic fractures can be a result of bone-weakening conditions like osteoporosis. If you have a disease that weakens your bones, engaging in regular activities or taking a small fall could result in a pelvic fracture. Diseases that weaken the bones can lead to pelvic fractures, which are typically stable fractures.
Athletic activities
Avulsion fractures of the pelvis can occur while playing sports, though they are less frequent. When a tendon or ligament separates from the bone to which it is attached, this occurs. A small piece of bone is lost when the tendon or ligament rips, along with it. An avulsion fracture of the pelvis is typically stable.
How to diagnose a pelvic fracture?
X-rays
Radiation is used in X-rays to create images of your bones. All pelvic fractures call for X-rays so your doctor can determine which part of your pelvis is broken, how minor or serious the fracture is, and how it should be treated.
CT scan
Several X-rays of your body are taken from various angles during a CT (computed tomography) scan to create detailed images. Compared to standard X-rays, a CT scan produces images that are more detailed. To learn more about your pelvic fracture and make sure you don’t have any additional injuries, your doctor may have you undergo a CT scan.
MRI
A large magnet, radio waves, and a computer are used in an MRI (magnetic resonance imaging) to create precise images of your organs and bones. If X-rays and a CT scan don’t reveal enough information about your fracture, your doctor may recommend that you get an MRI.
Surgical treatment of pelvic fracture
Usually, one or more surgeries are necessary to treat a more serious or unstable pelvic fracture. various procedures for pelvic fractures include:
External fixation
After a pelvic fracture, medical professionals use external fixation to stabilize your pelvic region. In this procedure, tiny incisions (surgical cuts) are made into your skin and muscle to insert metal pins or screws into your bones. On either side of your pelvis, pins and screws protrude from your skin and are connected to bars outside of your body by screws and pins. As your fracture(s) heal, the resulting system serves as a stabilizing frame to hold your broken bones in the right position.
Skeletal traction
A pulley system outside of your body called skeletal traction helps realign the fragments of broken bone (s). In order to help position your leg during skeletal traction, a surgeon inserts metal pins into your thigh bone or shinbone that protrude through your skin. The broken pelvic bone fragments are kept in a more normal position by weights attached to the pins that gently pull on your leg.
Open reduction and internal fixation
The displaced pelvic bone fragments are initially realigned into their proper positions prior to open reduction and internal fixation surgery. The pieces are then joined using metal plates or screws that are affixed to the bone’s exterior.
In a nutshell
For the fixation Pelvic Fractures, Zealmax Ortho is a trusted manufacturer of Orthopedic Implants which are available in a wide range of shapes & structures. All the orthopedic implants are available in high grade PEEK, SS & titanium materials.

